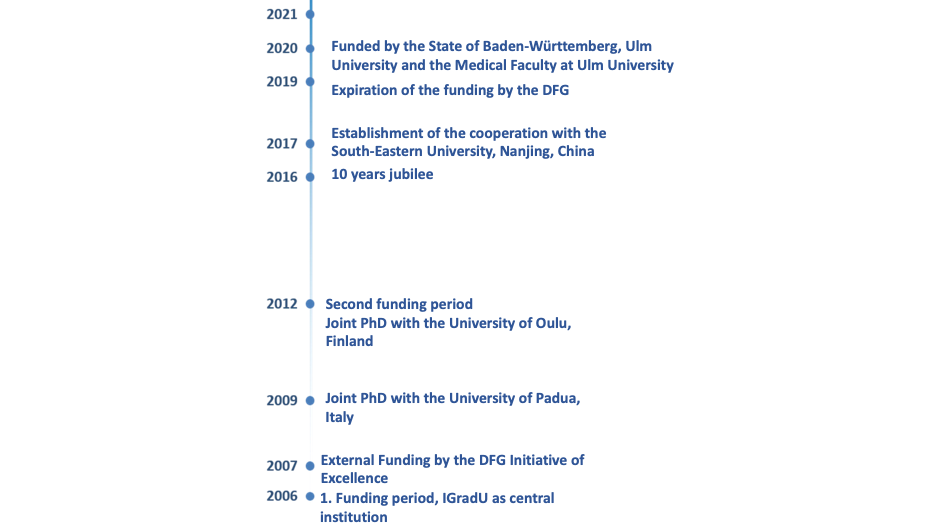
The International PhD programme in Molecular Medicine started in 2005 with only 7 students, funded by scholarships from the Medical Faculty of Ulm University. In 2007, IGradU was one of 45 Graduate Schools funded by the German Research Foundation (DFG). After several evaluations IGradU, who established and managed by Prof. Dr. Michael Kühl (Chairman) and PD Dr. Dieter Brockmann (managing director) until 2019, turned into a permanent structure at Ulm University funded by the DFG, the Ulm university and the medical faculty. In 2019, the DFG stopped funding graduate schools, so funding was secured by the State of Baden-Württemberg, Ulm University and the Medical Faculty at Ulm University.
What are our most important achievements and programs?
We have established six Research Training Groups (RTGs) covering the different topics in Molecular Medicine present at Ulm University. Each PhD student is supervised by a Thesis Advisory Committee (TAC) consisting of at least three members, one of whom comes from outside Ulm. IGradU is the umbrella organization for the training of PhD students from a large variety of collaborative research centres (SFBs) funded, for instance, by the DFG or the Federal Ministry of Education and Research (BMBF), such as the CRC1149 – Danger Response, Disturbance Factors and Regenerative Potential after Acute Trauma, CRC1074 – Experimental Models and Clinical Translation in Leukemia, and SyStaR – Molecular Systems Biology of Impaired Stem Cell Function and Regeneration during Aging, CRC 1279: Exploiting the Human Peptidome for Novel Antimicrobial and Anticancer Agents, CRC 1074: Experimental Models and Clinical Translation in Leukemia to mention just a few. We have enhanced our international outreach strategy by establishing several joint PhD programs with international Universities and by our guest professor programme. We have also implemented a diversity of gender programmes to support PhD students with children or female students during pregnancy. IGradU runs different mentoring programmes, including the well-known M4M-program (Mentoring for Molecular Medicine) in which senior citizens of Ulm offer support for our students and especially for those from abroad so that, from the time of their arrival in Germany until their disputation, these mentors can help to facilitate their integration into German society and culture. In addition, we have established a Junior Faculty to promote the scientific career of postdocs and group leaders.
How do we measure the success of our training programmes as well as that of the Graduate School? Of course, publications are only one side of the coin, and our students generally publish three to four papers in international peer-reviewed journals while completing their thesis. However, their future life and scientific career are of even more importance to us. We are proud that our alumni continue their career in well-known and highly ranked scientific institutions such as Harvard Medical School (USA), Stanford University School of Medicine (USA), Johns Hopkins (Baltimore, USA), McGill University (Canada), ETH Zürich (Switzerland) or Deutsches Krebsforschungszentrum DKFZ (Germany). Moreover, international global pharmaceutical companies, such as Boehringer Ingelheim and Roche, are also highly interested in our graduates.
Link to the beginnings and former cooperation...