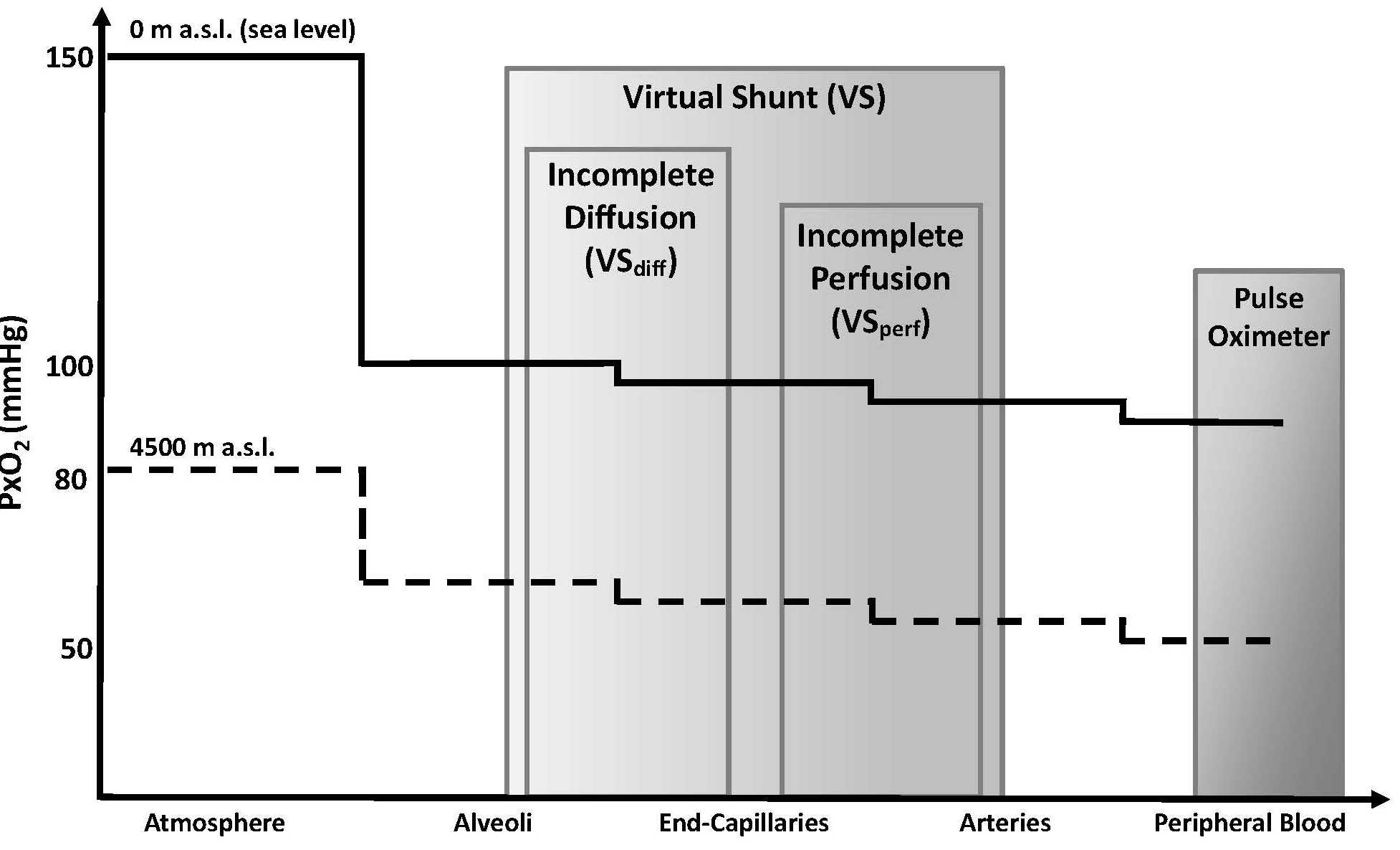
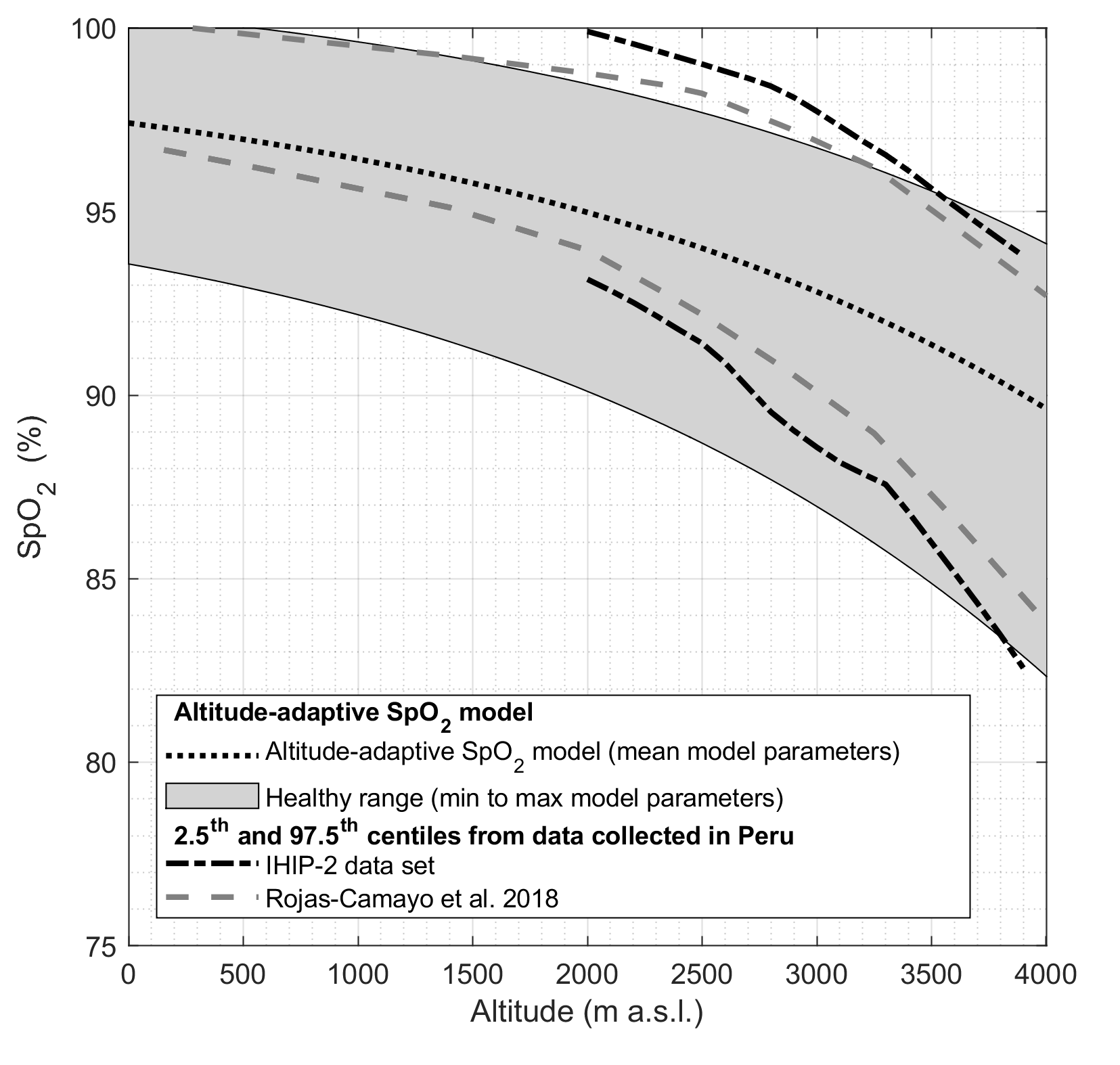
Normal oxygen saturation (SpO2) is dependent on altitude. We propose a computer model based on the oxygen cascade to predict SpO2 values between 0 and 4000 meters above sea level. The model was evaluated on pediatric permanent residents of Peru.
Tüshaus L, Moreo M, Zhang J, Hartinger SM, Mäusezahl D, Karlen W. Physiologically driven, altitude-adaptive model for the interpretation of pediatric oxygen saturation at altitudes above 2,000 m a.s.l. J Appl Physiol 127: 847–857, 2019. doi: 10.1152/japplphysiol.00478.2018