A01: Neuro-renal crosstalk as immune-modulator of trauma-related acute kidney injury and MODS
PI: M. Huber-Lang
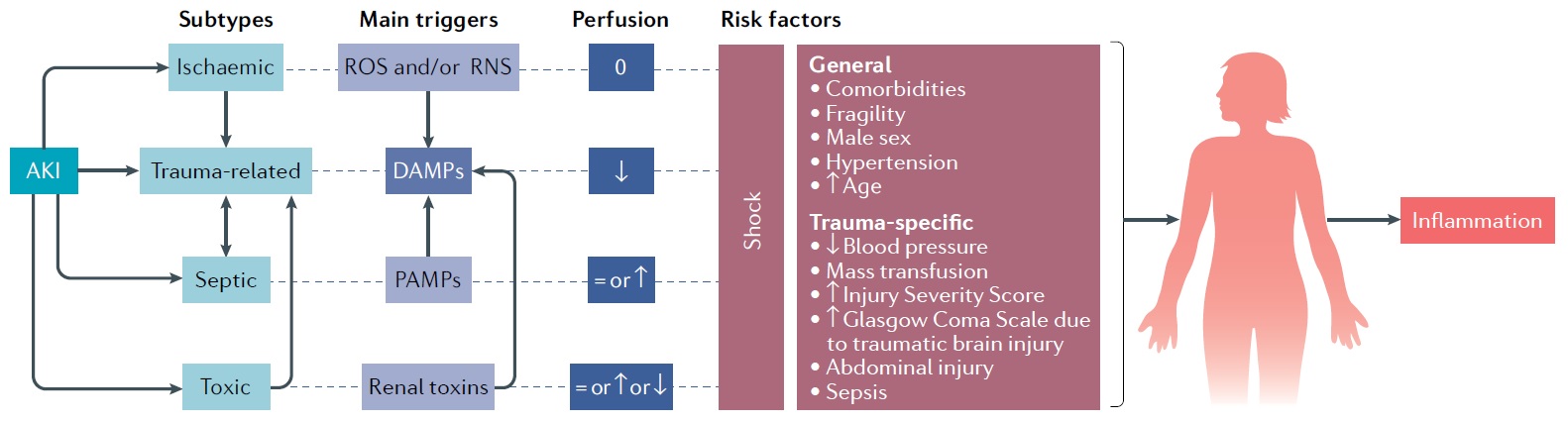
Trauma represents a global socioeconomic burden worldwide. The kidneys are a frequent remote target of a complex immuno-pathophysiological response resulting in trauma-related acute kidney injury (TRAKI). In the previous funding periods we identified hemorrhagic shock (HS) and associated alterations in the innate immunity including complement and leukocytes as major drivers of TRAKI and multi-organ dysfunction syndrome (MODS). Blocking central complement components appeared inefficient early after trauma/HS whereas some protective effects were evident during later stages regarding barrier dysfunction, TRAKI, and MODS. We also described upregulation of thirty-eight-negative kinase-1 in kidneys as one underlying molecular mechanism for renal damage after trauma/HS. The immune response appears to be an integral part of the post-trauma crosstalk between the kidneys, the nervous system and other organs, which can exacerbate MODS. However, little is known about the autonomous nerve system, vagal/sympathetic connections, and the impact of its functional balance in promoting and regulating the temporo-spatial renal response after trauma. Therefore, A01 hypothesizes i) that neurotransmitters significantly alter the response of kidney cells in a trauma micromilieu, ii) that the spatio-differential cellular and functional changes in kidneys during TRAKI and MODS can be improved by vagal stimulation as a therapeutic strategy, and iii) that the sympathetic/vagal imbalance contributes to perfusion-, immune-, and barrier-dysfunction in TRAKI and MODS. The data acquisition will employ an in vitro blood-urine-barrier model, murine trauma/HS with subsequent single cell RNAseq analysis of the kidneys, and intensive care unit patients after severe tissue injury monitored for their vagal activity, renal tissue perfusion, and multiple organ functions. Therefore, we expect to mechanistically characterize the neuro-renal crosstalk early after major trauma and to define a novel therapeutic concept to protect organs and particularly the vulnerable kidneys, and thus to improve the outcome post trauma.
Projektleiter
Prof. Dr. med. Markus Huber-Lang
Universitätsklinikum Ulm
Institut für Klinische und Experimentelle Trauma-Immunologie
Helmholtzstr. 8/1
89081 Ulm
Tel.: +49 731 500 54800
markus.huber-lang(at)uniklinik-ulm.de