C05: Role of ABCB5+ MSCs in niche homeostasis and repair after trauma
PI: K. Scharffetter-Kochanek
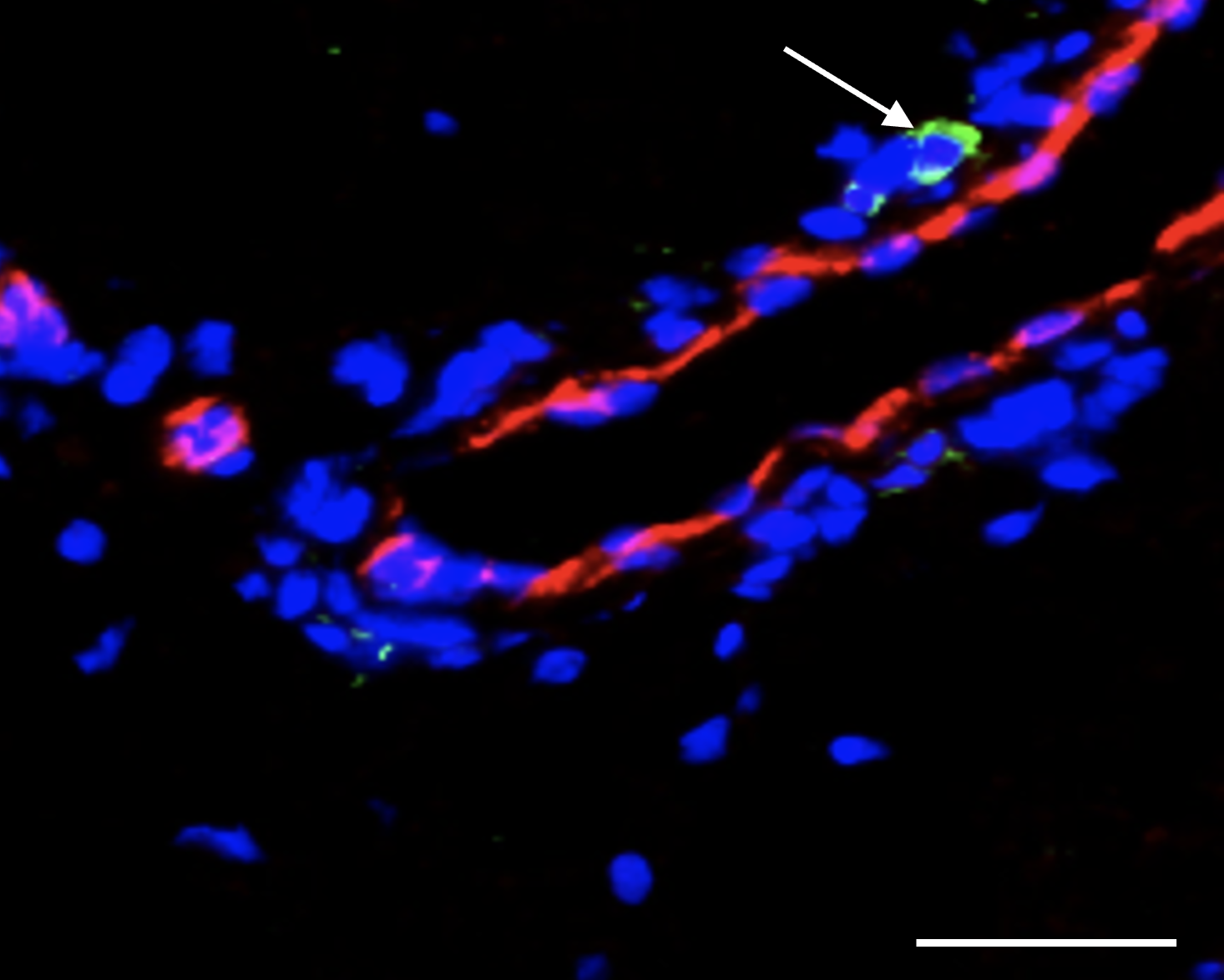
We uncovered that MSCs sense and shape their neighborhood at different trauma sites with accelerated tissue repair. Unexpectedly, chest trauma preceding skin injury led to accelerated wound healing of the skin. The overarching hypothesis of the next funding period is that in vivo priming of mesenchymal stem cells (MSCs) in their endogenous skin niches results in improved regenerative healing thereafter. This - we suggest - is due to a transient or long lasting epigenetic memory of the priming event in skin resident MSCs which upon subsequent wounding unleashes regenerative signaling events faster as opposed to unprimed MSCs. Three interrelated hypotheses will be explored: 1.) chest trauma primes MSCs with improved wound healing of the skin, 2.) trauma of other organs (brain, bone) enforces an adaptive skin response and enhances MSC functionality, 3.) direct priming of resident skin MSCs with in their endogenous niche with either S100A8/9 or preceding laser treatment promotes regenerative healing of subsequently induced full thickness skin wounds in mice and human volunteers. Finally, it remains to be elucidated whether priming MSCs in their endogenous skin niche results in reprogramming of their transcriptome and whether this is due to epigenetic changes with a “persisting memory” potentially unleashing the activation of transcription factors and target genes upon a subsequent skin trauma, eventually fostering faster regeneration. The decoding of mechanisms underlying endogenous MSC priming in murine and human skin in vivo will pave new therapeutic avenues to be translated in clinical routine.
Projektleiterin
Prof. Dr. med. Karin Scharffetter-Kochanek
Universitätsklinikum Ulm
Klinik für Dermatologie und Allergologie
Albert-Einstein-Allee 23
89081 Ulm
Tel.: +49 731 500 57501
Fax: +49 731 500 57502
karin.scharffetter-kochanek(at)uniklinik-ulm.de